





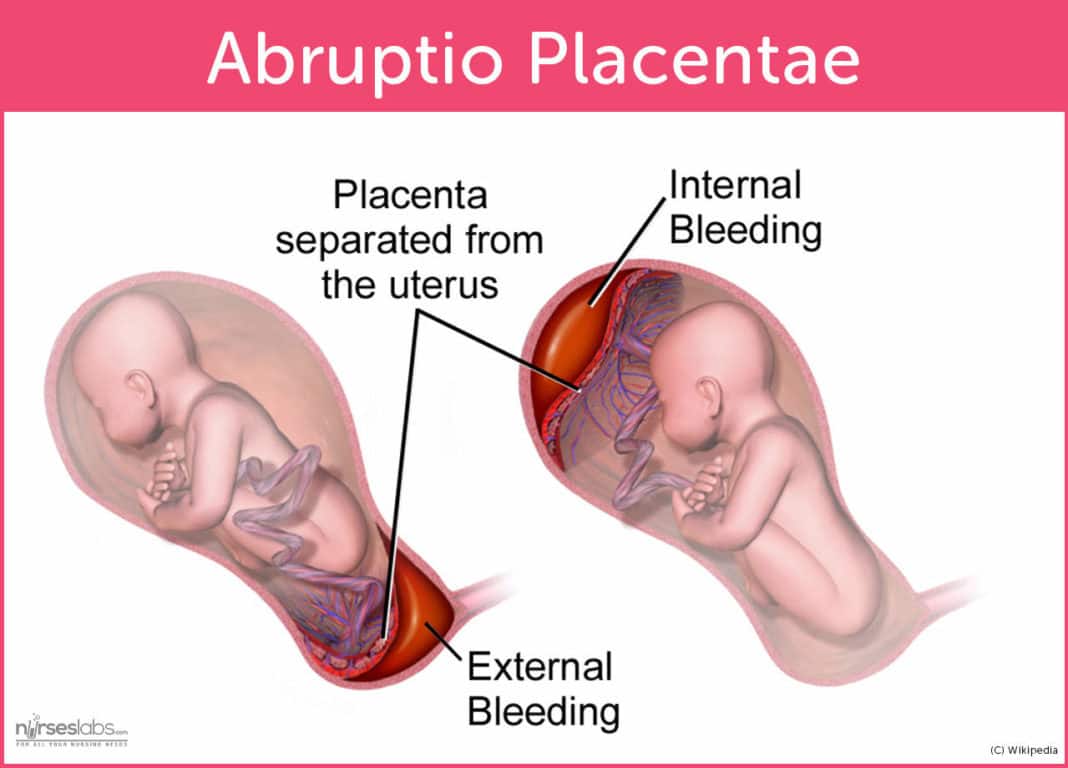
ABRUPTIO PLACENTA
Possible causes include trauma or injury to the abdomen — from an auto accident or fall, for example — or rapid loss of the fluid that surrounds and cushions the baby in the uterus (amniotic fluid).
CLINICAL MANIFESTATIONS
Vaginal bleeding.
Abdominal pain.
Back pain.
Uterine tenderness.
Uterine contractions.
PATHOPHYSIOLOGY
The placenta has implanted in the correct location.
For some unknown reasons, it suddenly begins to separate, causing bleeding.
This separation would occur late in pregnancy, and accounts for 10% of perinatal deaths.
DIAGNOSTIC TEST
Blood and urine tests
Ultrasound
Physical examination that includes palpation of the uterus
NURSING MANAGEMENT
Place the woman in a lateral, not supine position to avoid pressure in the vena cava.
Monitor fetal heart sounds.
Monitor maternal vital signs to establish baseline data.
Avoid performing any vaginal or abdominal examinations to prevent further injury to the placenta.
MEDICAL MANAGEMENT
Intravenous therapy. Once the woman starts to bleed, the physician would order a large gauge catheter to replace the fluid losses.
Oxygen inhalation. Delivered via face mask, this would prevent fetal anoxia.
Fibrinogen determination. This test would be taken several times before birth to detect DIC.
NURSING DIAGNOSIS
Deficient fluid volume related to bleeding during premature placental separationECLAMPSIA
Eclampsia is a known complication of preeclampsia during pregnancy and is associated with morbidity and mortality of both the mother and fetus if not properly diagnosed. Eclampsia is defined today as the new onset of generalized tonic-clonic seizures in a woman with preeclampsia. The progression of preeclampsia to eclampsia is sudden and without prediction.
Eclampsia is defined as the occurrence of one or more convulsions in a pre-eclamptic woman in the absence of any other neurological or metabolic causes.
Eclampsia is a severe complication of preeclampsia and poses both a risk to the mother and fetus. Eclampsia is a disease process that needs to be emergently identified and treated promptly.
It is an obstetric emergency affecting approximately 5/10,000 pregnancies, with a maternal mortality rate of 1.8% and a fetal mortality rate of up to 30%.
The majority of seizures occur in the postnatal period (44%), but they can also occur in the antepartum (38%) or intrapartum (18%) settings.
ETIOLOGY
The exact etiology of eclampsia is still unclear despite the advances in the understanding of preeclampsia. It is proposed that there is increased permeability of the blood-brain barrier during preeclampsia, which causes an alteration to cerebral blood flow due to impaired autoregulation.

CLINICAL MANIFESTATIONS
The hallmark feature of eclampsia is a new onset tonic-clonic type seizure, in the presence of pre-eclampsia (new onset hypertension and proteinuria after 20 weeks’ gestation).
The seizures typically last around 60 to 75 seconds, followed by a variable lasting post-ictal phase. Maternal convulsions may cause fetal distress and bradycardia.
Aside from the presence of seizures, the clinical presentation is much the same as that of pre-eclampsia, and often includes signs and symptoms relating to end-organ dysfunction:
Headache (usually frontal).
Hyper-reflexia.
Nausea and vomiting.
Generalized oedema.
Right upper quadrant pain +/- jaundice.
Visual disturbances e.g. flashing lights, blurred or double vision.
Change in mental stage
PATHOPHYSIOLOGY
Pathophysiology of preeclampsia and eclampsia is poorly understood. Factors may include poorly developed uterine placental spiral arterioles (which decrease uteroplacental blood flow during late pregnancy), a genetic abnormality, immunologic abnormalities, and placental ischemia or infarction. Lipid peroxidation of cell membranes induced by free radicals may contribute to preeclampsia.
DIAGNOSTIC TEST
Your obstetrician diagnoses eclampsia based on the presence of a seizure. They will perform an exam, blood work and regular blood pressure monitoring. They also order urine tests to look for increased protein in the urine.
Blood tests: Blood tests may show abnormal factors like red blood cell count or platelet count.
Urine tests: Urine tests typically show large amounts of protein in your urine.
Creatinine tests: Creatinine is a waste product that’s typically filtered out of your blood by your kidneys. Abnormally high levels of creatinine could be a sign of kidney failure.
Your healthcare provider will monitor the fetus and check its heart rate, movement, size and other factors through ultrasound to ensure it’s tolerating pregnancy well.
NURSING MANAGEMENT
Monitor blood pressure.
Assess fetal heart rate.
Send blood and urine for testing.
Administer prescribed medications.
Monitor reflexes on patients on magnesium sulfate.
Neurologic checks regularly.
Seizure precautions if ordered
MEDICAL MANAGEMENT
There are 5 main principles to address in the management of eclampsia, each of which are discussed in turn below.
1. Resuscitation
ABCDE assessment and intervention as appropriate.
Patients should lie in the left lateral position, with secured airway and oxygen therapy.
2. Cessation of Seizures
Eclamptic seizures are treated with magnesium sulphate (Table 4). The patient should be assessed for signs of hypermagnesaemia (hypo-reflexia, respiratory depression), and the fetus monitored via continuous CTG.
Note: Magnesium sulphate should be continued for 24 h after delivery/ last seizure, whichever is later.
3. Blood Pressure Control
The two most commonly used intravenous anti-hypertensives are labetalol and hydralazine. A target mean arterial pressure (MAP) of <120mmHg is used.
A rapid decrease in maternal blood pressure can cause fetal heart rate abnormalities. Therefore, continuous CTG monitoring is used during and for 30 minutes after giving IV anti-hypertensives.
4. Prompt Delivery of Baby and Placenta
The only definitive treatment of eclampsia is delivery of the fetus. However, the mother must be stable before delivery – with any seizures controlled, severe hypertension treated and hypoxia corrected. This is the case regardless of any fetal compromise.
Caesarean section is the ideal mode of delivery. However, intrapartum seizures in established labour may be managed by vaginal delivery.
After delivery, the patient will require HDU care until she is stable – well controlled blood pressure, adequate urine output, and discontinuation of MgSO4. This usually takes a minimum of 24 hours.
5. Monitoring
Fluid balance monitoring is important to prevent pulmonary oedema and detect acute kidney injury.
Indicators of complications of eclampsia should also be monitored – such as platelets, transaminases and creatinine levels.
NURSING DIAGNOSIS
The only way to prevent it is by early diagnosis and management. A good history and physical exam are essential for an accurate diagnosis. If signs and symptoms of preeclampsia are present, the patient should be seen every 4 hours until delivery. Any progress in signs or symptoms that would suggest changes in the condition should lead to more frequent assessments.
Perform actions to lessen the risk for seizures
Prevent maternal and fetal injuries if seizures occur
Monitor the signs of impending seizures
Psychological support to the woman and the family
References:
Eclampsia - Emergency Management - Risk Factors. (n.d.). TeachMeObGyn. Retrieved April 26, 2023
Magley, M., & Hinson, M. R. (2021). Eclampsia. PubMed; StatPearls Publishing.
Eclampsia: Causes, Symptoms, Diagnosis & Treatment. (n.d.). Cleveland Clinic.
Preeclampsia and Eclampsia - Gynecology and Obstetrics. (n.d.). MSD Manual Professional Edition.
ECTOPIC PREGNANCY
Ectopic pregnancy is implantation of a fertilized ovum in a site other than the endometrial lining of the uterus. This occurs when a fertilized egg implants in a location that can’t support its growth and it can rarely occur in the ovary and abdominal cavity or cervix. An ectopic pregnancy happens when a fertilized egg implants outside of the uterus, most commonly in the fallopian tube (95%)
Moreover, the other common site of ectopic pregnancy are the following such as:
Fimbrial - 8%
Interstitial - 8%
Ampulla – 80%
Isthmic – 12%
Cervical
Abdominal
Tubo-ovarian
ETIOLOGY
In most cases, conditions that slow down or block the movement of the egg down the fallopian tube cause ectopic pregnancy. This could happen due to:
The scar tissue, adhesions or inflammation from a prior pelvic surgery.
Fallopian tubes have damage, such as from a sexually transmitted infection (STI)
Born with an irregularly-shaped fallopian tube.
Having a growth blocking in the fallopian tube.
CLINICAL MANIFESTATIONS
The early symptoms of an ectopic pregnancy can be very similar to typical pregnancy symptoms. However, the patient may experience additional symptoms during an ectopic pregnancy, including:
Vaginal bleeding.
Amenorrhea
Dizziness or weakness.
Pain in the lower abdomen, pelvis and lower back.
If the fallopian tube ruptures, the pain and bleeding could be severe enough to cause additional symptoms. These can include:
Fainting.
Shoulder pain.
Low blood pressure (hypotension)
Rectal pressure or bowel problems.
Moreover, when a tube bursts, the patient may feel sudden, sharp lower abdominal pain and this is a medical emergency.
PATHOPHYSIOLOGY
An ectopic pregnancy happens when a fertilized egg implants outside of your uterus.
The egg is meant to travel down your fallopian tubes and embed itself into the wall of your uterus, where it can develop.
Anatomic distortion and obstruction of the fallopian tube are widely responsible for most ectopic implantations. In an ectopic pregnancy, the egg implants in one of the structures along the way.
It lodges on that constricted part and implantation takes place at that area instead of the uterus.
DIAGNOSTIC TEST:
Tests to determine the possibility of ectopic pregnancy must be performed first before the diagnosis.
PELVIC ULTRASOUND: An early pregnancy ultrasound is the most common determinant of an ectopic pregnancy.
MAGNETIC RESONANCE IMAGING: This is also another way to detect the presence of ectopic pregnancy
HYSTEROSALPINGOGRAPHY: ALSO KNOWN AS UTEROSALPINGOGRAPHY is a radiologic procedure to investigate the shape of the uterine cavity and the shape and patency of the fallopian tube
NURSING MANAGEMENT
Nurses must also have their own function when it comes to ectopic pregnancy, even without a direct order from the physician. These may include:
Assessing the vital signs to establish baseline data and determine if the patient is under shock.
Maintaining accurate intake and output to establish the patient’s renal function.
Upon the arrival at the emergency room, place the woman flat in bed.
MEDICAL MANAGEMENT
The medical management of a woman with an ectopic pregnancy should be initiated the moment she is brought to the emergency room. These can include:
Administration of methotrexate: Methotrexate is a chemotherapeutic agent that is a folic acid antagonist. It destroys rapidly growing cells such as the trophoblast and the zygote. This would be administered until a negative hCg titer result has been produced.
Administration of mifepristone: An abortifacient that causes sloughing off of the tubal implantation site. Both of these therapies would leave the tube intact and no surgical scarring.
Intravenous therapy :This would be performed when the ectopic pregnancy has already ruptured to restore intravascular volume due to bleeding.
Withdrawing of blood sample :A large amount of blood would be lost, so blood typing and crossmatching must be done in anticipation of a blood transfusion. The blood sample would also be used to determine the hemoglobin levels of the pregnant woman.
Moreover, surgical interventions would be performed after the rupture of the ectopic pregnancy to ensure that the reproductive system would still be functional and no complications would arise.
Laparoscopy: This will be performed to ligate the bleeding blood vessels and repair or remove the damaged fallopian tube.
Salpingectomy: This intervention would be performed if the fallopian tube is completely damaged. The affected tube would be removed and what would be left would be sutured appropriately.
NURSING DIAGNOSIS
The care provider should do a complete observation to diagnose any possible causes of ectopic pregnancy such as:
Risk for Deficient Fluid Volume: related to bleeding from a ruptured ectopic pregnancy.
Powerlessness: related to early loss of pregnancy secondary to ectopic pregnancy.
References
GESTATIONAL ANEMIA
ETIOLOGY
Dietary factors (insufficient iron intake) Chronic blood loss from Gl bleeding.
Impaired Gl absorption of iron (prolonged diarrhea, gastrectomy) Increased iron requirements (rapid body growth, menstruation, pregnancy).
Iron-refractory deficiency anemia (IRIDA)
PATHOPHYSIOLOGY
The body stores of iron decreases as do the stores of transferrin which binds and transports iron. This leads to depletion of red blood cells, resulting in decreased hemoglobin concentration and decreased oxygen-carrying capacity of the blood.
DIAGNOSTIC TEST
Complete blood count (CBC) in the first trimester is recommended for all pregnant women to screen for anemia. The screening of pregnant women for IDA in absence of anemia is still debatable. If IDA is suspected, a ferritin level of <30 ng/ml is diagnostic.
NURSING MANAGEMENT
Administer prescribed medications which includes iron supplements (IV, IM, or oral)
Advise patients to take iron supplements an hour before meals for maximum absorption.
Advise patients to take liquid forms of iron using a straw to prevent teeth staining.
MEDICAL MANAGEMENT
Medical care starts with establishing the diagnosis and reason for the iron deficiency.
Iron therapy. Oral ferrous iron salts are the most economical and effective medication for the treatment of iron deficiency anemia; of the various iron salts available, ferrous sulfate is the one most commonly used.
Diet. The addition of nonheme iron to national diets has been initiated in some areas of the world.
NURSING DIAGNOSIS
Fatigue related to decreased hemoglobin and diminished oxygen-carrying capacity of the blood.
Deficient knowledge related to the complexity of treatment, lack of resources, or unfamiliarity with the disease condition.
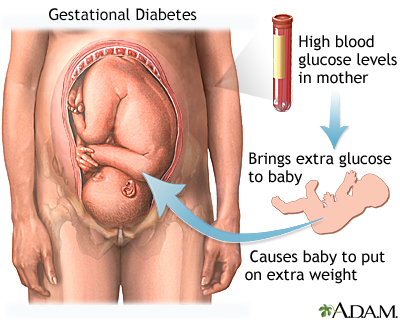
GESTATIONAL DIABETES
ETIOLOGY
If your body is unable to produce enough additional insulin during pregnancy, gestational diabetes will develop. the body can use the hormone insulin, which is produced in the pancreas, to help utilize glucose as fuel and regulate blood sugar levels. Your body produces unique hormones and experiences other changes during pregnancy, such as weight growth. Insulin resistance is the result of these alterations, which cause your body's cells to poorly utilize insulin. Throughout their late pregnancy, all pregnant women experience some insulin resistance. Some pregnant women are unable to produce enough insulin to reverse insulin resistance, but most can. Pregnant diabetics are born to these women.
CLINICAL MANIFESTATIONS
Glycosuria on two successive office visits
Recurrent monilial vaginitis
Macrosomia of the fetus on ultrasound
Polyhydramnios
PATHOPHYSIOLOGY
1. In gestational diabetes mellitus (type III, GDM), insulin antagonism by placental hormones, human placental lactogen, progesterone, cortisol, and prolactin leads to increased blood glucose levels. The effect of these hormones peaks at about 26 weeks’ gestation. This is called the diabetogenic effect of pregnancy.
2. The pancreatic beta cell functions are impaired in response to the increased pancreatic stimulation and induced insulin resistance.
3. Pregnancy complicated by diabetes puts the mother at increased risk for the development of complications, such as spontaneous abortion, hypertensive disorders, and preterm labor, infection, and birth complications.
4. The effects of diabetes on the fetus include hypoglycemia, hyperglycemia, and ketoacidosis. Hyperglycemic effects can include:
Congenital defects
Macrosomia
Intrauterine growth restriction
Intrauterine fetal death
Delayed lung maturity
Neonatal hypoglycemia
Neonatal hyperbilirubinemia
DIAGNOSTIC TEST
Fasting blood sugar test will reveal elevated blood glucose levels.
A 50-g glucose screen (blood glucose level is measured 1 hour after client ingests a 50-g glucose drink) reveals elevated blood glucose levels. The normal plasma threshold is 135 to 140 mg/dL.
NURSING MANAGEMENT
1. Establish an initial database and maintain serial documentation of test results throughout the pregnancy.
2. Provide client and family teaching.
3. Arrange for the client to consult with a dietitian to discuss the prescribed diabetic diet and to ensure adequate caloric intake
4. Address emotional and psychosocial needs. Intervene appropriately to allay anxiety regarding diabetes and childbirth.
5. Prepare the client for intensive frequent intrapartum assessment, which may include:
Fetal monitoring
Intravenous infusion of glucose, insulin, and oxytocin
Evaluation for diabetic ketoacidosis (signs and symptoms include altered level of consciousness, labored breath sounds, fruity breath odor, and ketonuria)
Intravenous fluid and electrolyte replacement therapy
Invasive maternal cardiac monitoring
MEDICAL MANAGEMENT
Treatment for gestational diabetes aims to keep blood glucose levels equal to those of pregnant women who don't have gestational diabetes. The treatment always includes special meal plans and scheduled physical activity, and it may also include daily blood glucose testing and insulin injections.
NURSING DIAGNOSIS
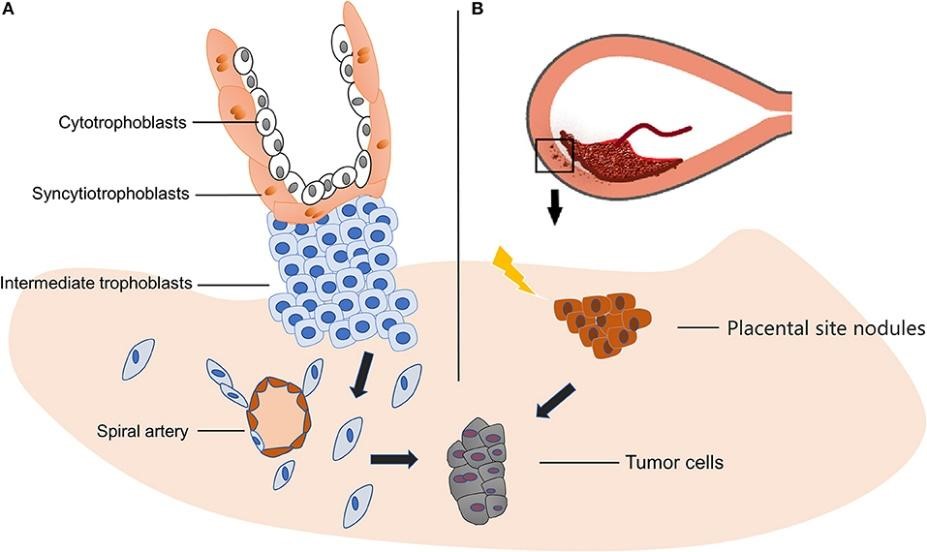
Gestational Trophoblastic Disease
Gestational trophoblastic disease is the degeneration and abnormal proliferation of the trophoblastic villi. The cells become filled with clear fluid, giving them the appearance of grape-like vesicles.
ETIOLOGY
The most common types of gestational trophoblastic disease occur when a sperm cell fertilizes an empty egg cell or when two sperm cells fertilize a normal egg cell. Your risk is higher based on your:
Age: Gestational trophoblastic disease occurs in women of childbearing age.
History of molar pregnancy
Prior miscarriage(s) or problems getting pregnant
Blood type: Women with blood types A or AB are at slightly higher risk than those with types B or O.
Diet: A few studies have found that a low level of beta-carotene in the diet may be linked with a higher risk of molar pregnancy. More research is needed to confirm this connection.
CLINICAL MANIFESTATION
If you have gestational trophoblastic disease, you may not notice any signs or symptoms and your pregnancy may seem normal. Your doctor may notice signs of the disease during your routine prenatal care visits. Possible signs include:
Uterus expands faster than normal. Because the trophoblast cells proliferate abnormally, it does so in such a rapid pace that the uterus reaches its growth landmarks before the usual time.
Vaginal bleeding. When the H-mole is still not identified at the 16th week of pregnancy, it will identify itself through vaginal bleeding accompanied by clear fluid filled vesicles.
A larger-than-normal uterus or swollen abdomen
PATHOPHYSIOLOGY
Fertilization occurs as the sperm enters the ovum. In instances of a partial mole, two sperms might fertilize a single ovum.
Reduction division or meiosis was not able to occur in a partial mole. In a complete mole, the chromosome undergoes duplication.
The embryo fails to develop completely. There are 69 chromosomes that develop for the partial mole, and 46 chromosomes for the complete mole.
The trophoblastic villi start to proliferate rapidly and become fluid-filled grape-like vesicles.
DIAGNOSTIC TEST
Diagnostic tests are ordered to check for a presence that might indicate a positive gestational trophoblastic disease.
Pregnancy test. This may not be able to detect specifically the H-mole, but this will confirm if the woman is pregnant or not.
CT scan - CT scans use X-rays to create cross-sectional pictures of your abdominal area. They are useful in showing the size of the tumor, if lymph nodes are swollen, and if the tumor has spread to other organs.
PET scan - An imaging test that can help reveal the metabolic or biochemical function of your tissues and organs. The PET scan uses a radioactive drug called a tracer to show both typical and atypical metabolic activity.
NURSING MANAGEMENT
Nurses must also take action during the critical stages of the pregnancy. We must be able to function on our own while waiting for any orders from the physician.
Assess the abdominal girth of the pregnant woman to check if it is within the usual landmark of pregnancy.
Assess for signs and symptoms of pregnancy induced hypertension, because for a woman with H-mole, they occur earlier than the 20th week of pregnancy.
Instruct the woman to save all perineal pads containing any clots or tissue that has passed out of her during bleeding.
MEDICAL MANAGEMENT
The physician would order medications and other interventions that would ensure the safety of the woman during this complicated period.
Methotrexate: Physicians may order a prophylactic course of methotrexate, which attacks rapidly growing cells like the abnormally growing trophoblastic cells.
Dactinomycin: This is ordered by the physician once metastasis occurs.
NURSING DIAGNOSIS
Grieving be related to:
loss of pregnancy
anger
social detachment
GOAL: Resolves feelings about the loss.
References
Belleza, M. (2016, December 22). Gestational Trophoblastic Disease. Retrieved from Nurseslabs:
Cancer.Net. (2022, July 22). Gestational Trophoblastic Disease: Symptoms and Signs.
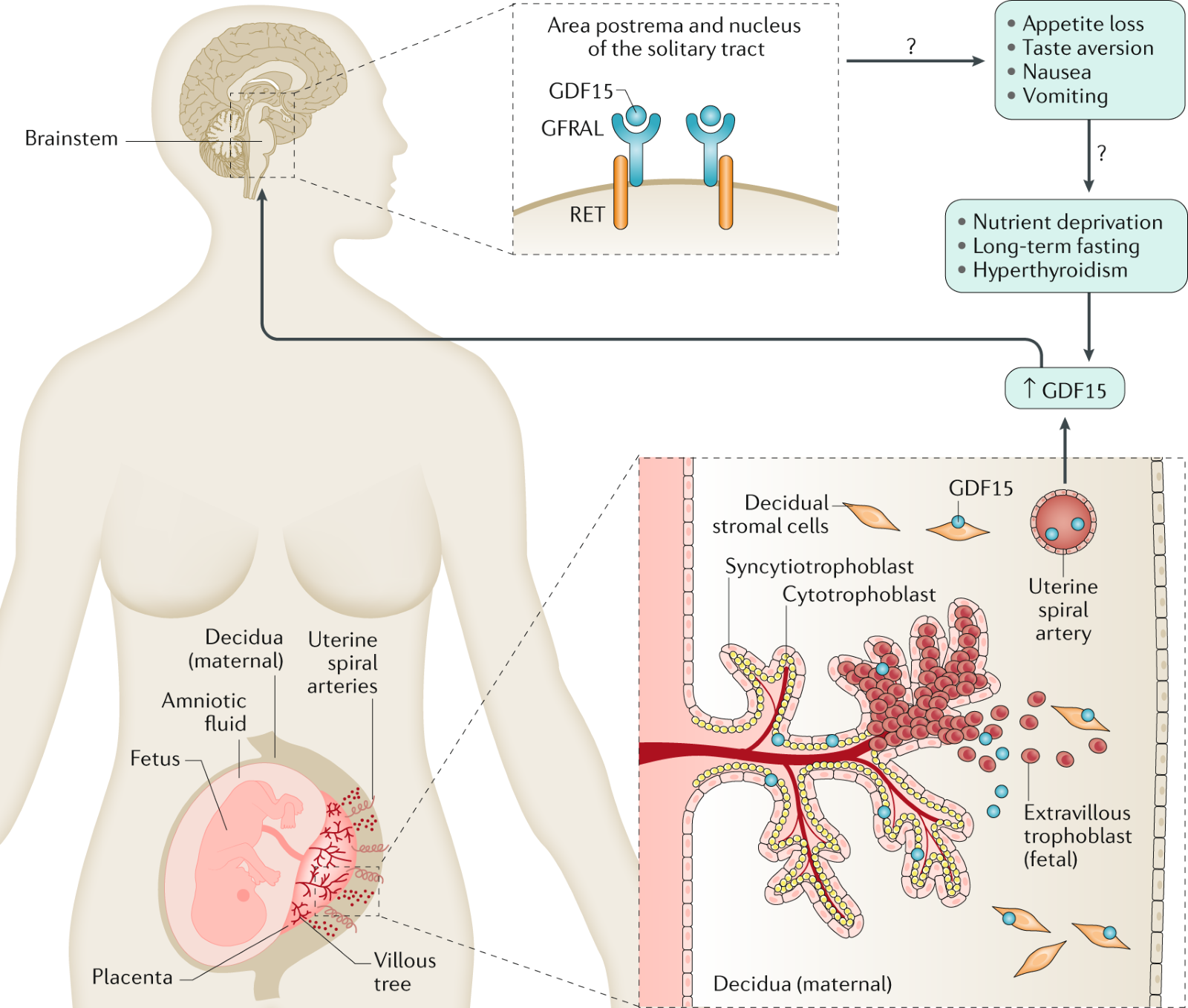
HYPEREMESIS GRAVIDANUM
Nausea and vomiting is a common occurrence in pregnancy, with at least 70 percent of women experiencing some form of it. It’s typically referred to as morning sickness, though it can happen at any time of day. But sometimes the symptoms are so extreme — severe, persistent nausea, vomiting, and weight loss during pregnancy — that it may be diagnosed as a less common disorder known as hyperemesis gravidarum. Hyperemesis gravidarum can lead to dehydration and nutrient loss, affecting both the health of a pregnant woman and the fetus she’s carrying. Nausea can be debilitating, interfering with daily activities and quality of life. It usually subsides at between 14 and 20 weeks (about 4 and a half months) of gestation. Women with hyperemesis gravidarum have an increased risk of preterm birth, preeclampsia, and eclampsia — a rare complication of preeclampsia that causes seizures during pregnancy — among other issues, but the risk is low.
ETIOLOGY
The etiology of hyperemesis gravidarum is largely unknown, but several theories exist (see pathophysiology). There are, however, risk factors associated with the development of hyperemesis during pregnancy. Increased placental mass in the setting of a molar or multiple gestations has been associated with a higher risk of hyperemesis gravidarum. Additionally, women who experience nausea and vomiting outside of pregnancy due to the consumption of estrogen-containing medications, exposure to motion, or have a history of migraines are at higher risk of experiencing nausea and vomiting during pregnancy. Some studies also suggest a higher risk of hyperemesis in women with first-degree relatives, for instance, if her mother or sister experienced hyperemesis gravidarum.
Experts don’t know for sure what causes hyperemesis gravidarum. However, rising hormone levels are most likely what causes it. Specifically, HCG (human chorionic gonadotropin), which your body makes during pregnancy — very quickly and in large amounts. HCG levels peak around 10 weeks of pregnancy, which is when most people report having the most severe symptoms. Estrogen, another hormone that increases during pregnancy, may also play a role in causing nausea and vomiting.
CLINICAL MANEFISTATIONS
The defining symptoms of hyperemesis gravidarum are gastrointestinal in nature and include nausea and vomiting. Other common symptoms include ptyalism (excessive salivation), fatigue, weakness, and dizziness. This vomiting can lead to:
Feeling dizzy, lightheaded, and faint
Losing more than 5 percent of body weight
Becoming dehydrated, with signs of dehydration such as dark urine and dry skin
PATHOPHYSIOLOGY
The exact cause of hyperemesis gravidarum remains unclear. However, there are several theories for what may contribute to the development of this disease process.
Hormone Changes: Levels of human chorionic gonadotropin (HCG) have been implicated. HCG levels peak during the first trimester, corresponding to the typical onset of hyperemesis symptoms. Some studies show a correlation between higher HCG concentrations and hyperemesis. However, this data has not been consistent.
Changes in the Gastrointestinal System: It is well-known that the lower esophageal sphincter relaxes during pregnancy due to the elevations in estrogen and progesterone. This leads to an increased incidence of gastroesophageal reflux disease (GERD) symptoms in pregnancy, and one symptom of GERD is nausea. Studies examining the relationship between GERD and emesis in pregnancy report conflicting results.
Genetics: An increased risk of hyperemesis gravidarum has been demonstrated among women with family members who also experienced hyperemesis gravidarum.
NURSING MANAGEMENT
1. Promote resolution of the complication.
2. Address emotional and psychosocial needs. Maintain a non-judgmental atmosphere in which the client and family can express concerns and resolve some of their fears.
MEDICAL MANAGEMENT
If you have severe symptoms of hyperemesis gravidarum, you may need to be hospitalized. Hyperemesis gravidarum is the second leading cause of hospitalization in early pregnancy. For less severe cases, you may be able to seek treatment at home or at a doctor’s office. While the course of treatment for hyperemesis gravidarum varies from person to person, your doctor may recommend one or more of the following:
Vitamin B6
Small, frequent meals that include dry, bland foods such as crackers
NURSING DIAGNOSIS
Nausea: Nausea is an uneasiness of the stomach that often comes before vomiting. Vomiting is the forcible voluntary or involuntary emptying ("throwing up") of stomach contents through the mouth.
Related to:
Pregnancy
Unpleasant sensory stimuli
Rise in hormone levels
Multiple gestation pregnancy
Genetic predisposition
As evidenced by:
Food aversion
Increased salivation
Gagging sensation
Sour taste
Increased swallowing
Vomiting
Expected outcomes:
Patient will verbalize the reduction of incidence and severity of nausea and vomiting.
Patient will demonstrate effective interventions that can help alleviate nausea and vomiting.
Patient will be able to eat small meals and/or consume fluids.
INCOMPETENT CERVIX
ETIOLOGY
A condition that refers to the inability of the cervix to hold the fetus any longer until term because it has dilated prematurely.
Uterine abnormalities and genetic disorders affecting a fibrous type of protein that makes up your body's connective tissues (collagen) might cause an incompetent cervix.
CLINICAL MANIFESTATION
Show. This is a pink-tinged vaginal fluid that is discharged from the vaginal opening as a sign that the cervix has dilated. Increased pelvic pressure. The fetus is already descending, causing a pressure felt by the mother on her pelvis. Cervical dilation. Upon inspection of the physician, the cervix would show dilation
NURSING INTERVENTIONS
Determine any factors that further contribute to the anxiety of the woman so it could be avoided.
Monitor vital signs to determine any physical responses of the patient that could affect her condition.
Convey empathy and establish a therapeutic relationship to encourage client to express her feelings.
Provide accurate information about the situation to help client back into reality.
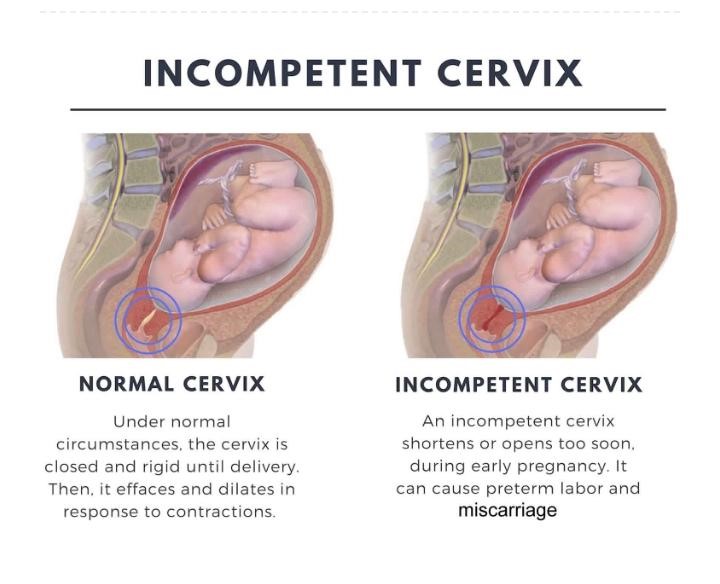
PATHOPHYSIOLOGY
When the fetus reaches its 20th week, it starts to become heavy and gain fats.
The mother’s cervix is weak, and it could not hold the fetus’ weight anymore as it slowly starts to dilate.
This would cause the appearance of a show, a pink-tinged vaginal discharge.
Then, the membranes would rupture and amniotic fluid would be discharged.
Uterine contractions would start followed by a short labor, then the birth of the fetus.
DIAGNOSTIC TESTS
There are few diagnostic tests that could detect an incompetent cervix before it usually happens. It is usually diagnosed after the pregnancy has already been lost.
Ultrasound. This is the only test that the physician could order if an incompetent cervix is already suspected.
NURSING MANAGEMENT
As nurses, here is what we could do to help in our own way.
MEDICAL MANAGEMENT
Medical management by the physician would not include any medications that could hinder the dilation of the cervix. Surgical procedures are immediately enforced to prevent compromising the pregnancy.
NURSING DIAGNOSIS
Anxiety related to impending loss of pregnancy as evidenced by premature dilation of the cervix.
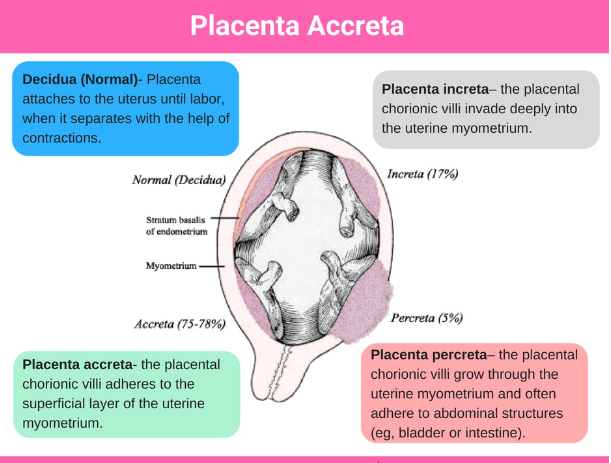
PLACENTA ACCRETA
Placenta accreta is an uncommon condition in which the chorionic villa adheres to the myometrium. It can be exhibited as:
Placenta accreta: the placental chorionic villi adheres to the superficial layer of the uterine myometrium.
Placenta increta: the placental chorionic villi invade deeply into the uterine myometrium.
Placenta percreta: the placental chorionic villi grow through the uterine myometrium and often adhere to abdominal structures (eg, bladder or intestine).
ETIOLOGY
Predisposing factors are prior uterine surgery and placenta previa
CLINICAL MANIFESTATIONS
Placenta fails to separate
Profuse hemorrhage may result depending on the portion of placenta involved.
PATHOPHYSIOLOGY
Implantation in an area of defective endometrium with no zone separation between the placenta and the myometrium.
DIAGNOSTIC TEST
Ultrasound
MRI
Note: Your health care provider can evaluate how deeply the placenta is implanted in your uterine wall.
MEDICAL MANAGEMENT
Placenta accreta is a rare condition and is associated with considerable maternal morbidity and mortality. Though the surgical approach of hysterectomy is a definitive therapy, there are occasions when conservation of the uterus is desired by the patient.
NURSING DIAGNOSIS
Risk for bleeding
Related to:
Disease process
Low-lying placenta
Sexual intercourse
Vaginal examinations
Labor
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms, as the problem has not occurred yet and nursing interventions are directed at the prevention of symptoms.
Expected Outcomes:
The patient discusses and demonstrates precautions to prevent bleeding complications
The patient is able to deliver the fetus without excessive bleeding
References
AWagrier M. (2022, October 21) Nurse Together Placenta Previa Nursing Diagnosis & Care Plan
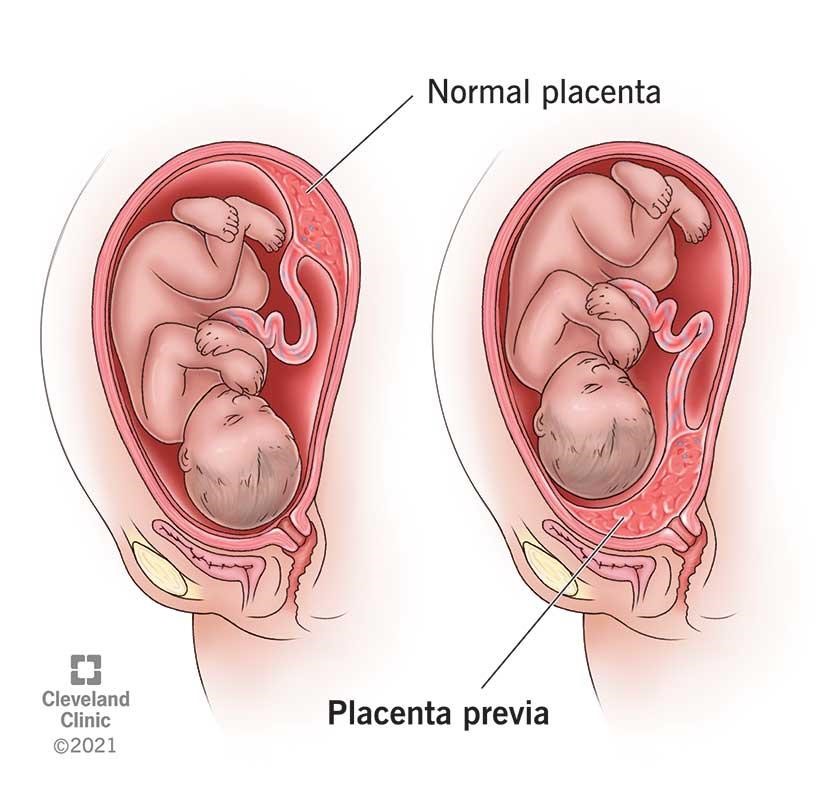
PLACENTA PREVIA
The placenta has implanted at the bottom of the uterus, over the cervix or close by, which means the baby can’t be born vaginally.
ETIOLOGY
Low implantation of the fertilised egg
Abnormalities of the uterine lining, such as fibroids
Scarring of the uterine lining (endometrium)
Abnormalities of the placenta
Multiple babies, such as twins
Multiple pregnancies - a woman who has already had six or more deliveries has a risk of one in 20.
CLINICAL MANIFESTATION
Painless vaginal bleeding - During the later stages of pregnancy, the bottom part of the uterus thins and spreads to accommodate the growing baby. If the placenta is anchored to the bottom of the uterus (as occurs with placenta previa), this thinning and spreading separates the placenta and causes bleeding.
Sexual intercourse can also cause bleeding from the placenta previa in later pregnancy. During labour, the cervix thins and dilates, which would normally allow the baby to exit into the vagina. In placenta previa, the dilation of the cervix further tears the placenta and causes bleeding.
PATHOPHYSIOLOGY
The placenta implants on the lower part of the uterus.
The lower uterine segment separates from the upper segment as the cervix starts to dilate.
The placenta is unable to stretch and accommodate the shape of the cervix, resulting in bleeding.
DIAGNOSTIC TEST
Ultrasound scan
Feeling the mother’s belly to establish the baby’s position (the baby is sideways or presenting bottom-first in around one in three cases of placenta previa)
NURSING MANAGEMENT
Assess baseline vital signs especially the blood pressure. The physician would order monitoring of the blood pressure every 5-15 minutes.
Assess fetal heart sounds to monitor the wellbeing of the fetus.
Monitor uterine contractions to establish the progress of labor of the mother.
MEDICAL MANAGEMENT
Medical interventions are necessary to ensure that the safety of both mother and fetus are still intact.
Intravenous therapy: This would be prescribed by the physician to replace the blood that was lost during bleeding.
Avoid vaginal examinations: This may initiate hemorrhage that is fatal for both the mother and the baby.
Attach external monitoring equipment: To monitor the uterine contractions and record fetal heart sounds, an external equipment is preferred than the internal monitoring equipment.
NURSING DIAGNOSIS
Fear related to outcome of pregnancy due to bleeding.
POSTPARTUM DEPRESSION
Postpartum depression (PPD) is a type of depression that affects new mothers after giving birth. It typically occurs within the first few weeks to months after delivery, but can develop at any time during the first year postpartum.
ETIOLOGY
The exact cause of postpartum depression (PPD) is not fully understood, but it is likely a combination of biological, psychological, and environmental factors. Some of the factors that may contribute to the development of PPD include:
1. Hormonal changes: During pregnancy, a woman's hormone levels, particularly estrogen and progesterone, increase significantly.
2. Genetics: Women with a family history of depression or other mood disorders may be at a higher risk for developing PPD.
3. Stressful life events: The transition to motherhood can be challenging, and women who experience significant stress during pregnancy or after childbirth, such as financial stress, relationship problems, or a difficult birth experience, may be more likely to develop PPD.
4. Lack of social support: Women who do not have adequate social support during and after pregnancy may be more vulnerable to developing PPD.
5. Previous history of depression: Women who have experienced depression or other mental health conditions in the past are at a higher risk for developing PPD.
CLINICAL MANIFESTATION
Postpartum depression (PPD) can manifest in a variety of ways, and symptoms may vary from person to person. Some common clinical manifestations of PPD include:
1. Mood changes: This may include feelings of sadness, irritability, anxiety, or hopelessness that are persistent and do not improve with time.
2. Sleep disturbances: Women with PPD may have difficulty sleeping or may sleep excessively.
3. Appetite changes: This may include a loss of appetite or an increase in appetite.
4. Fatigue and loss of energy: Women with PPD may feel extremely tired and have difficulty completing daily tasks.
PATHOPHYSIOLOGY
The exact pathophysiology of postpartum depression (PPD) is not fully understood, but it is believed to involve complex interactions between hormonal, genetic, environmental factors, and changes in brain function and structure.
1. Hormonal: After childbirth, hormone levels drop rapidly, which may contribute to the development of PPD
2. Environmental factors: Stress, lack of social support, and a history of trauma may also contribute to the development of PPD.
3. Changes in brain function and structure: Studies have shown that women with PPD have altered activity in certain areas of the brain, particularly in areas involved in emotional processing and regulation.
DIAGNOSTIC TEST
There is no single test to diagnose postpartum depression (PPD): Dagnosis is typically made based on clinical evaluation, which may include a physical exam, review of symptoms, and assessment of medical history and family history.
Edinburgh Postnatal Depression Scale (EPDS): Commonly used screening tool that can help healthcare providers identify women who may be at risk for PPD.
NURSING MANAGEMENT
Nursing management of postpartum depression (PPD) may include:
1. Assessing for risk factors: Nurses should assess for risk factors for PPD, including a history of depression or anxiety, a lack of social support, a difficult pregnancy or childbirth experience, and a history of trauma.
2. Educating the patient: Nurses should provide education to new mothers about PPD, including its symptoms, risk factors, and available treatments.
3. Providing emotional support: Nurses should provide emotional support to new mothers who are experiencing PPD, including active listening, validation of feelings, and empathy.
MEDICAL MANAGEMENT
Medical management of postpartum depression (PPD) may include:
1. Medication: Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help alleviate symptoms of PPD.
2. Psychotherapy: Psychotherapy, such as cognitive-behavioral therapy (CBT) or interpersonal therapy (IPT), may be recommended to help new mothers manage symptoms of PPD and develop coping strategies.
3. Hormone therapy: In some cases, hormone therapy may be used to help regulate hormone levels and improve mood.
4. Referral to a specialist: Patients with severe or treatment-resistant PPD may be referred to a mental health specialist, such as a psychiatrist or psychologist, for further evaluation and treatment.
5. Support groups: Support groups or peer counseling may be recommended to help new mothers with PPD connect with others who are experiencing similar challenges.
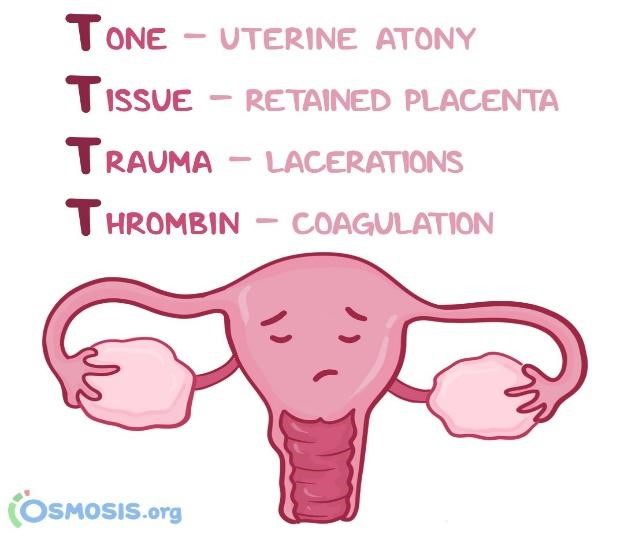
POSTPARTUM HEMORRHAGE
ETIOLOGY
Postpartum hemorrhage has four main: uterine atony, trauma, retained placenta, and coagulopathy. The most common and challenging to treat is uterine atony, where a lack of uterine contractility leads to massive hemorrhage postpartum.
CLINICAL MANIFESTATION
Heavy vaginal bleeding.
Drop in blood pressure or signs of shock.
Tense and rigid uterus.
Inadequate blood coagulation.
PATHOPHYSIOLOGY
There are different main causes of postpartum hemorrhage, and they cause bleeding in different ways.
In uterine atony, the uterus stops contracting, which leads to bleeding because the placental sites have closed.
If the uterus has retained placental fragments, it can also cause massive bleeding postpartum.
DIAGNOSTIC TEST
Pelvic exam: Your provider checks your vagina, uterus, and cervix
Hematocrit: This is a blood test that checks the percent of your blood (called whole blood) that’s made up of red blood cells.
Ultrasound: Your provider can use ultrasound to check for problems with the placenta or uterus. Ultrasound is a test that uses sound waves and a computer screen to make a picture of your baby inside the womb or your pelvic organs.
NURSING MANAGEMENT
Need to intervene early or during the course of a hemorrhage to help the patient regain her strength and vitality.
Establish data that would give essential care to the patient with hemorrhage.
Address emotional and psychosocial needs.
Save all perineal pads used during bleeding and weigh them to determine the amount of blood loss.
Blood Replacement
NURSING DIAGNOSIS
Deficient fluid volume related to excessive bleeding after birth.
Risk for Infection.
Ineffective Tissue Perfusion
ADHD (Attention-deficit/Hyperactivity disorder)
One of the most prevalent neurodevelopmental diseases in children is ADHD. It frequently persists into maturity and is typically first diagnosed in infancy. Children with ADHD may struggle to focus, manage impulsive behaviors (doing without considering the consequences), or be extremely active.

ETIOLOGY
Recent research relates genetic causes to ADHD. Scientists are researching additional potential causes and risk factors, such as brain injury, in addition to genetics. environmental dangers (like lead) being exposed when pregnant or when young.
MANIFESTATIONS
Easily Distracted
Daydreaming
Forgetfulness
Excessive Talking
Careless Mistakes
Impatience
NURSING INTERVENTIONS
Accept the child or individual as what he is
Approach the child at his current level of functioning
Use simple and direct instructions.
Implement scheduled routine every day
Avoid stimulating or distracting settings
Give positive reinforcements
Encourage physical activity
PATHOPHYSIOLOGY
ADHD is linked to cognitive and functional problems. In those with ADHD, it is discovered that the anterior cingulate gyrus and the dorsolateral prefrontal cortex (DLFPC) are tiny.
NURSING MANAGEMENT
Nurses must possess the necessary expertise to care for patients with ADHD, and they must take behavioral and environmental factors into account.
MEDICAL MANAGEMENT
The therapeutic approach to ADHD has been shifting.
Behavioral psychotherapy: When combined with a successful pharmaceutical regimen, behavioral psychotherapy is frequently beneficial; behavioral therapy or behavior modification programs can assist reduce ambiguous expectations and improve organization.
Psychosocial interventions: Effective psychosocial interventions include behavioral parent training and behavioral classroom management, which work best when combined with psychopharmacological methods.
Cognitive therapy for adults with ADHD: Through the use of cognitive and behavioral therapy principles and techniques to improve time management, adult ADHD patients are now better equipped to combat the anxiety and depressive symptoms that interfere with task performance.
NURSING DIAGNOSIS
Defective Coping
Impaired social interactions
Altered thought processes
Risk for parental role conflict
Risk for injury
Risk for delay in growth and development
ATRIAL SEPTAL DEFECT (ASD)
An abnormal opening in the atrial septum between the right and the left atria often caused by failure of foramen ovale to close.
ETIOLOGY
Every child is born with an opening between the upper heart chambers. It’s a normal fetal opening that allows blood to detour away from the lungs before birth. After birth, the opening is no longer needed and usually closes or becomes very small within several weeks or months.
Sometimes the opening is larger than normal and does not close after birth. Some children can have other heart defects along with Atrial Septal Defect (ASD).
In some cases, the tendency to develop ASD might be inherited (genetic). Genetic syndrome can cause extra or missing pieces of chromosomes that can be associated with ASD.
In most children the cause is not known. The exact cause of ASD is unknown.
CLINICAL MANIFESTATIONS
Manifestations depend on its size and its location Usually asymptomatic: small to moderate size and may not be diagnosed until preschool years or later. Children with larger, more severe ASDs, might have some of these signs or symptoms:
Shortness of breath, especially during physical activity.
Extreme tiredness
Palpitations or rapid heartbeat
Cyanosis, a bluish tint to the skin or lips due to decreased oxygenation.
Delayed growth and development in infants and children.
Frequent respiratory infections
Harsh systolic murmur.
Hypertrophy of the right side of the heart.
Congestive heart failure may occur depending on the size of the defect.
PATHOPHYSIOLOGY
The pathophysiology of ASD involves abnormal blood flow between the atria, which can lead to increased pressure and volume overload in the right atrium and the right ventricle.
Normally, oxygen-poor blood returns from the body to the right atrium and is then pumped into the right ventricle, which pumps it to the lungs for oxygenation. Oxygen-rich blood from the lungs returns to the left atrium and is then pumped into the left ventricle, which pumps it to the rest of the body.
In the case of ASD, there is a hole in the atrial septum, allowing blood to flow from the left atrium to the right atrium, instead of the normal unidirectional flow. As a result of the abnormal blood flow, there is increased blood volume in the right atrium and right ventricle, which cause the right side of the heart to work harder that normal, which can eventually lead to right ventricular hypertrophy (thickening of the right ventricular wall).
The increased volume in the right atrium and ventricle can also cause increased pressure in these chambers. Over time, this pressure can cause pulmonary hypertension (high blood pressure in the pulmonary arteries), which can lead to right heart failure.
Blood shunting from left to right can also lead to oxygen-rich blood being pumped back to the lungs, which can lead to an increased workload on the lungs, in some cases, to Eisenmenger syndrome, which is characterized by the development of pulmonary hypertension and a reversal of the shunt from right to left, resulting in cyanosis.
The severity of ASD and its impact on the heart and lungs depend on the size and location of the defect, as well as the age at which it is diagnosed and treated. Early diagnosis and intervention can prevent or minimize the potential complications associated with ASD.
DIAGNOSTIC TEST
Electrocardiogram (ECHO)
Echocardiogram (ECG/EKG)
Chest X-ray
Cardiac catheterization
Magnetic resonance imaging (MRI),
NURSING MANAGEMENT
Assess and monitor vital signs frequently, including heart rate, blood pressure, and oxygen saturation to detect any changes or signs of complications. Promote rest and activity limitation. Nurse can educate patient about the importance of rest and activity limitations, and help them develop strategies to conserve energy.
Administer medications as prescribed, such as diuretics to manage symptoms like fluid overload. Ensure medications are administered on schedule and monitor for any adverse effects. Provide emotional support and health education.
Monitor for potential complications. Prepare client for surgery or interventional procedures. Provide education about the procedure and postoperative care, as well as assist with preoperative preparation and postoperative monitoring.
After surgery:
Closely monitor vital signs, central venous and intra-arterial pressures, intake and output.
Give an antibiotic and an analgesic, as ordered.
MEDICAL MANAGEMENT
Medication to treat symptoms, namely diuretics will be attempted first in an effort to allow the defect to close spontaneously.
Defect that remain 5 mm or greater with persistent shunting after an observation period should be referred for closure to decrease the incidence of supraventricular dysrhythmias and prevent pulmonary vascular disease. Secundum ASD, defect that is located in the center of the atrial septum, is typically closed in the catheterization lab with a device that sits in the defect space.
Cardiac Catheterization, a thin, flexible tube (a catheter) is inserted into a blood vessel in the leg that leads to the heart. A special implant is positioned into the hole and is designed to flatten against the septum on both sides to close and permanently seal the ASD. Taking a low dose of aspirin for 6 months is needed to prevent the risk of blood clots. Less physical activity for a few days or weeks.
Sinus venosus, found high in the septum where the pulmonary veins enter the left atrium, and primum defects, found low in the atrial septum near the inferior vena cava (IVF), are referred for surgical closure, they cannot be closed in the catheterization lab because of their anatomy. When the ASD is very large or too close to the wall of the heart, surgery is needed to close the defect. Surgical closure involves a median sternotomy incision and cardiopulmonary bypass.
NURSING DIAGNOSIS
Risk for decreased cardiac output related to the defect structure.
Impaired gas exchange related to decreased pulmonary blood flow secondary to shunting of blood from the right atrium to the left atrium through the ASD.
Risk for injury related to the risk of stroke or embolism due to the shunting of blood through the ASD.
References:
American Heart Association. (2019). Atrial septal defect (ASD).
Straight Nursing. (n.d). Atrial septal defect nursing assessment and intervention.
AUTISM
Autism spectrum disorder (ASD) is a developmental disability caused by differences in the brain. People with ASD often have problems with social communication and interaction, and restricted or repetitive behaviors or interests. People with ASD may also have different ways of learning, moving, or paying attention.
ETIOLOGY
Autism spectrum disorder has no single known cause. Given the complexity of the disorder, and the fact that symptoms and severity vary, there are probably many causes. Both genetics and environment may play a role.
GENETICS: Several different genes appear to be involved in autism spectrum disorder. For some children, autism spectrum disorder can be associated with a genetic disorder, such as Rett syndrome or fragile X syndrome. For other children, genetic changes (mutations) may increase the risk of autism spectrum disorder. Still other genes may affect brain development or the way that brain cells communicate, or they may determine the severity of symptoms. Some genetic mutations seem to be inherited, while others occur spontaneously.
ENVIRONMENTAL FACTORS: Researchers are currently exploring whether factors such as viral infections, medications or complications during pregnancy, or air pollutants play a role in triggering autism spectrum disorder.
PATHOPHYSIOLOGY
1. Dysfunction of neural functions: Some findings on the pathophysiology of autism are based on the brain’s ability to perform neural functions efficiently. Our brain’s neural function is best assessed based on its ability to build healthy neural circuits, and this is granted by a process called synaptic pruning. A synapse is the point on a nerve that transmits information from one neuron to the next. A synapse allows for neural communication between cells. When there’s too many synaptic connections, the brain goes through a process of cutting down; known as synaptic pruning.
2. Genetic and epigenetics factors in autism: Epigenetics is the study of how the environment and our behaviors affect how our genes work. Although epigenetic changes are reversible, and do not change your DNA sequence, they can however change your body reads a DNA sequence. In addition, some epigenetic changes can be hereditary.
3. The endocrine system: The endocrine system consists of glands that secrete hormones, namely: the thyroid gland, the parathyroid glands, the hypothalamus, pituitary gland, and pineal gland in the brain, the thymus, the pancreas, ovaries (in women), and testes (in men), and the adrenals.
DIAGNOSTIC TESTS
Autism Diagnosis Interview – Revised (ADI-R) A clinical diagnostic instrument for assessing autism in children and adults.
Autism Diagnostic Observation Schedule – Generic (ADOS-G)
Childhood Autism Rating Scale (CARS)
Gilliam Autism Rating Scale – Second Edition (GARS-2)
NURSING MANAGEMENT
1. The nurse must be able to familiarize the combination of symptoms associated with autism of the patient.
2. The nurse is the coordinator of therapies and interventions that meet the specific needs of individual children.
3. During the treatment session, the nurse’s main goal is to provide safety. The nurse must ensure that unnecessary may harm the child, and are removed from the area. It is also important to let the other staff members know of the child’s special needs.
4. Apply appropriate behavioral strategies. One example is the applied behavioral analysis (ABA). This program uses a one-on-one teaching approach that reinforces the practice of various skills. The goal is to get the child close to normal developmental functioning.
5. Listen to the child, his parents and the caregivers. As a nurse, you have to be an effective channel of communication among these people.
MEDICAL MANAGEMENT
Special education for the child
Behavioral management
Medications
Biomedical and complementary therapies
Antipsychotic drugs
Minerals, vitamins and dietary interventions
NURSING DIAGNOSIS
Impaired verbal communication related to reduced ability to read body language
At risk for injury
Impaired social interaction
Family and caregiver lack of knowledge regarding autism
Ineffective therapeutic regimen related to economic difficulties
CEREBRAL PALSY
Cerebral palsy is a group of disorders that affect normal movement in different parts of the body. This condition can cause problems with posture, manner of walking (gait), muscle tone, and coordination of movement. The word “cerebral” refers to the brain’s cerebrum, which is the part of the brain that regulates motor function. “Palsy” describes the paralysis of voluntary movement in certain parts of the body. There are several types of cerebral palsy that are characterized by the location of the brain injury. Symptoms can vary depending on where and how badly the brain was damaged. The types of cerebral palsy include:
Ataxic cerebral palsy: This type is caused by cerebellum damage resulting in issues with motor control and movement.
Athetoid/dyskinetic cerebral palsy: Caused by basal ganglia and/or cerebellum damage; symptoms include fluctuating muscle tone and involuntary movements.
Hypotonic cerebral palsy: This rare type, also caused by cerebellum damage, is characterized by floppy muscles, excess flexibility, and poor mobility.
Spastic cerebral palsy: The most common type of cerebral palsy, caused by damage to the motor cortex or pyramidal tracts and characterized by tight muscles and jerking movements.
Mixed cerebral palsy: Multiple areas of brain damage can cause patients to have more than one type of cerebral palsy.

ETIOLOGY
Cerebral palsy is caused by damage or abnormal development in the parts of the brain that control movement. These events can happen before, during, or shortly after birth or in the first few years of life, when the brain is still developing. In many cases the exact cause of cerebral palsy is not known.
CLINICAL MANEFISTATIONS
The symptoms of cerebral palsy vary from person to person and range from mild to severe. Some people with cerebral palsy may have difficulty walking and sitting. Other people with cerebral palsy can have trouble grasping objects. The effects of the condition can become more or less obvious or limiting as a child grows and develops motor skills. They also vary depending on the part of the brain that was affected.
Developmental delay. History of gross motor developmental delay in the first year of life.
Abnormal muscle tone. The most frequently observed symptom; the child may present as either hypotonic or, more commonly, hypertonic, with either decreased or increased resistance to passive movements, respectively; children with cerebral palsy may have an early period of hypotonia followed by hypertonia; a combination of axial hypotonia and peripheral hypotonia is indicative of a central process.
PATHOPHYSIOLOGY
Cerebral palsy (CP), defined as a group of nonprogressive disorders of movement and posture, is the most common cause of severe Neurodisability in children. Understanding its physiopathology is crucial to developing some protective strategies. Interruption of oxygen supply to the fetus or brain asphyxia was classically considered to be the main causal factor explaining later CP. However, several ante-, peri-, and postnatal factors could be involved in the origins of CP syndromes. Congenital malformations are rarely identified. CP is most often the result of environmental factors, which might interact with genetic vulnerabilities, and could be severe enough to cause the destructive injuries visible with standard imaging (i.e., ultrasonographic study or MRI), predominantly in the white matter in preterm infants and in the gray matter and the brainstem nuclei in full-term newborns. Moreover, they act on an immature brain and could alter the remarkable series of developmental events. Biochemical key factors originating in cell death or cell process loss, observed in hypoxic-ischemic as well as inflammatory conditions, are excessive production of proinflammatory cytokines, oxidative stress, maternal growth factor deprivation, extracellular matrix modifications, and excessive release of glutamate, triggering the excitotoxic cascade. Only two strategies have succeeded in decreasing CP in 2-year-old children: hypothermia in full-term newborns with moderate neonatal encephalopathy and administration of magnesium sulfate to mothers in preterm labor.
DIAGNOSTIC TEST
A doctor will diagnose cerebral palsy by taking a complete medical history, performing a physical exam that includes a detailed neurological exam, and evaluating the symptoms. The following additional testing may also be used:
Electroencephalogram (EEG). An EEG is used to evaluate electrical activity in the brain. A doctor may order it when someone is showing signs of epilepsy, a primary cause of seizures. Learn more about epilepsy and seizures.
MRI. An MRI uses powerful magnets and radio waves to produce detailed images of the brain. A healthcare professional may perform an MRI in order to identify brain irregularities or injuries.
CT scan. A CT scan creates clear, cross-sectional images of the brain. It can also reveal brain damage.
Ultrasound. A cranial ultrasound is a method of using high-frequency sound waves to get basic images of a young infant’s brain. It’s relatively quick and inexpensive. Learn more about ultrasound.
Blood tests. A healthcare professional may take and test a sample of blood to rule out other possible conditions, such as bleeding disorders.
NURSING MANAGEMENT
Use of communication board or computer-assisted communication
Self-care is the goal of care for children
Provide adequate nutrition and rest
Increase calorie intake
Maintain a safe environment
Provide headgear or padded bed
NURSING DIAGNOSIS
Based on the assessment data, the major nursing diagnoses include:
Risk for injury related to spasms, uncontrolled movements, and seizures.
Impaired physical mobility related to spasms and muscle weakness.
Changes in growth and development related to neuromuscular disorders.
Impaired verbal communication related to difficulty in articulation.
Risk for aspiration related to neuromuscular disorders.
Disturbed thought processes related to cerebral injury, learning disabilities.
Self-care deficit is related to muscle spasms, increased activity, cognitive changes.
Deficient knowledge related to home care and therapeutic needs.
CLEFT LIP AND PALATE
ETIOLOGY
Cleft lip occurs as a familial tendency or most likely occurs from the transmission of multiple genes. It is twice as prevalent in the Japanese population and occurs rarely. A formation may be aided by teratogenic factors present during weeks 5 to 8 of intrauterine life, such as viral infection or possibly a deficiency of folic acid.
Most cases appear to be consistent with the concept of multifactorial inheritance as evidenced by an increased incidence in relatives and monozygotic twins
Environmental. In some cases, babies inherit a gene that makes them more likely to develop a cleft, and then an environmental trigger actually causes the cleft to occur.

CLINICAL MANIFESTATIONS
These defects are readily apparent at birth.
Cleft lip involves a notched upper lip border, nasal distortion, and may include unilateral or bilateral involvement.
Cleft palate is a visible or palpable gap in the uvula, soft palate, hard palate, and/or incisive foramen with exposed nasal cavities and associated nasal distortion.
Difficulty swallowing. The newborn has a hard time in swallowing, with the potential for liquids or foods to come out the nose.
PATHOPHYSIOLOGY
During embryonic development the lateral and medial tissues forming the upper lip fuse between weeks 7 and 8 of gestation; the palatal tissues forming the hard and soft palate fuse between 7 and 12 weeks of gestation.
Cleft lip and cleft palate result when these tissues fail to fuse
The cleft may be a simple notch in the vermilion line, or it may extend up into the floor of the nose.
DIAGNOSTIC TEST
Cleft lip may be detected by a sonogram while the infant is in utero. If not detected then, it is readily apparent on inspection at birth.
Cleft palate can be determined by depressing the newborn’s tongue with a tongue blade. This reveals the total palate and the extent of the cleft palate. Be sure to have clear lighting to visualize the palate clearly.
NURSING MANAGEMENT
Assess for problems with feeding, breathing, parental bonding, and speech.
Ensure adequate nutrition and prevent aspiration.
Provide special nipples of feeding devices (e.g., soft pliable bottle with soft nipples with enlarged opening) for a child unable to suck adequately on standard nipples.
Hold the child in a semi-upright position; direct the formula away from the cleft and toward the side and back of the mouth to prevent aspiration.
Feed the infant slowly and burp frequently to prevent excessive swallowing of air and regurgitation.
NURSING DIAGNOSIS
Risk for aspiration related to a reduced level of consciousness after surgery.
Risk of injury to the operative site related to newborns' desire to suck thumb or fingers and anatomical changes.
Imbalanced nutrition less than body requirement related to food intake
Deficient knowledge (mother) regarding proper feeding techniques
COLIC
Colic is paroxysmal abdominal pain that generally occurs in infants under 3 months of age. Colic is most common during the first 6 weeks of life. It is also when a healthy baby cries for a very long time, for no obvious reason. In most infants, colic disappears almost magically at 3 months of age, probably because it becomes easier to digest foods and an infant maintains a more upright position by this time which allows less gas to form
ETIOLOGY
The exact cause of Colic is still unclear. However, some potential causes why it happens are being explored. These include:
Having a milk allergy or intolerance
Being sensitive to gas
Unable to calm themselves
CLINICAL MANIFESTATIONS
Colic often begins suddenly, with loud and mostly nonstop crying like a colicky crying. It is louder with a high-pitched, and more urgent sounding than regular crying. Colicky babies can be very hard to calm down. Moreover, babies with colic are often fussy and gassy. The face of the infants with colic becomes red and flushed. If offered a bottle, the infant will suck vigorously for a few minutes a s if starved, then stop as another wave of intestinal pain occurs. Additionally, colic is defined as when a baby’s crying lasts for more than 3 hours a day, happens more than 3 days a week, and occurs for more than 3 weeks. Babies who have colic may also show manifestations such as:
Burping often or passing a lot of gas
Having a tight belly
Curling up their legs toward their belly when crying
Clenching their fists when the abdomen become tense.
PATHOPHYSIOLOGY
It may occur in susceptible infants from overfeeding or from swallowing too much air while feeding
Formula-fed babies are more likely to have colic than breast-fed babies possibly because they swallow more air while drinking or because formula is harder to digest.
DIAGNOSTIC TEST
Thorough assessment of the signs and symptoms of colic that may be present to the infant.
Observe the duration and frequency of the problem (usually lasts up to 3 hours a day and occurs at least 3 days every week)
A family medical history is also important to obtain because allergy to milk may stimulate colic.
Thorough history taking on the feeding practices of the baby and the preparation of the mother.
Blood tests and X-rays or other imaging tests may be done (these can help find out if your baby has other health problems)
NURSING MANAGEMENT
Ask parents about the duration of the problem and its frequency.
Ask what happens just before the attack and describe the attack itself.
Document the number and type of bowel movements.
Determine the baby’s feeding pattern.
Offering a pacifier may be comforting.
Help parents plan relief time from infant care to relieve stress.
NURSING DIAGNOSIS:
The care provider should do a complete physical exam to diagnose any possible causes for the baby's distress. The exam will include:
Measuring baby's height, weight and head circumference
Listening to the heart, lungs and abdominal sounds
Examining the limbs, fingers, toes, eyes, ears and genitals
Assessing reaction to touch or movement
Looking for signs of rash, inflammation, or other signs of infection or allergies

ConnectED is dedicated to providing information and support for families facing high-risk pregnancy and infant-related issues. This platform is designed to be a comprehensive resource for families seeking guidance, advice, and education on a wide range of topics related to maternal and infant health.
Our platform offers a range of services and resources that are tailored to meet the specific needs of families. We provide in-depth information on a variety of topics, including diseases' clinical manifestations, etiologies, pathophysiology, diagnostics tests, management, and medications needed. Our site also connects families with experienced healthcare professionals who specialize in high-risk pregnancy and infant care. Through our network of medical experts, families can receive personalized support and guidance to help them navigate the challenges of pregnancy and early childhood.
In addition to our educational and support resources, we offer a range of tools and services to help families manage their healthcare needs. These include access to online appointment scheduling, medical records, and personalized health plans.
Overall, ConnectED is a valuable resource for families facing high-risk pregnancy and infant-related issues. We are committed to providing comprehensive education, support, and guidance to help families ensure the best possible maternal and infant health outcomes.

ConnectED: Connecting Families to Information and Education was created in order to help families regarding health care of motherhood and the development of childhood which shows significant events in the life of a parent. Gathering high risk and most common diagnosed cases of the pregnant baby and its baby that shows things that will help them to prevent and can maintain their healthy lifestyle.
ConnectED: Connecting Families to Information and Education is an education that provides information for both people and nurses that serves as relevant information regarding high risk diseases in the obstetrics and pediatrics cases.

OBJECTIVES
To offer the mothers and parents a platform to source answers, knowledge, and guidance for high risk conditions that affect infants, children, adolescence and mothers.
To provide open, free, and relevant information to people about maternal and pediatric diseases.
To serve as an important source of nurses in updating themselves which helps them in the state of art practice of nursing.
To offer the mothers and parents a platform to source answers, knowledge, and guidance for high risk conditions that affect infants, children, adolescence and mothers.